Pediatric cancer prediction has entered a transformative era, thanks to advancements in artificial intelligence in pediatric oncology. Innovative predictive AI tools are being developed to process multiple MRI scans, enabling healthcare professionals to assess glioma recurrence risk with remarkable precision. A recent Harvard study highlighted how these AI-driven solutions surpass traditional methods that have long governed relapse prediction in children diagnosed with brain tumors. By leveraging extensive datasets and sophisticated algorithms, the potential for tailored children cancer treatment has never been greater. With early and accurate predictions, families can navigate the complexities of pediatric cancer care with improved confidence and reduced anxiety.
The realm of children’s cancer prognosis is advancing rapidly, particularly through the integration of AI technologies. These predictive models utilize advanced analytics to evaluate the likelihood of cancer recurrence in young patients, significantly enhancing diagnostic accuracy. By focusing on historical imaging data, such as MRI scans in pediatric patients, researchers are uncovering deeper insights into the behavior of tumors like gliomas. This paradigm shift not only facilitates a more personalized treatment approach but also optimizes the overall care journey for affected children. As such, innovations in this field promise to transform the landscape of pediatric oncology.
The Role of AI in Pediatric Oncology
Artificial intelligence (AI) is revolutionizing the field of pediatric oncology by providing tools that improve diagnostic accuracy and treatment strategies. In particular, recent advancements have focused on the use of AI to predict cancer recurrence in child patients. Studies have shown that AI algorithms analyzing MRI scans can detect subtle changes over time, indicating potential relapse long before traditional methods may pick up on these signs. By harnessing the power of predictive AI tools, health professionals can significantly improve outcomes for young patients with cancers such as pediatric gliomas.
With AI in pediatric oncology, the promise is clear: providing tailored care plans that directly respond to the unique needs of each child. The ability to analyze vast amounts of imaging data allows for more informed decision-making regarding treatment approaches like surgery or adjuvant therapies. AI tools not only enhance risk assessment but also foster more efficient use of medical resources, ultimately leading to a more humane and less stressful experience for families navigating the complexities of children’s cancer treatment.
Predicting Glioma Recurrence Risk in Children
The prediction of glioma recurrence in pediatric patients has historically presented a significant challenge for oncologists. Traditional methods rely heavily on single-image analysis which can miss critical signs due to the complex nature of tumor behavior in children. However, recent AI innovations utilizing temporal learning have changed the landscape, allowing for the evaluation of multiple MRI scans over time. This methodological leap has resulted in significantly better predictive accuracy regarding recurrence risk, thereby optimizing follow-up care protocols for children recovering from brain tumors.
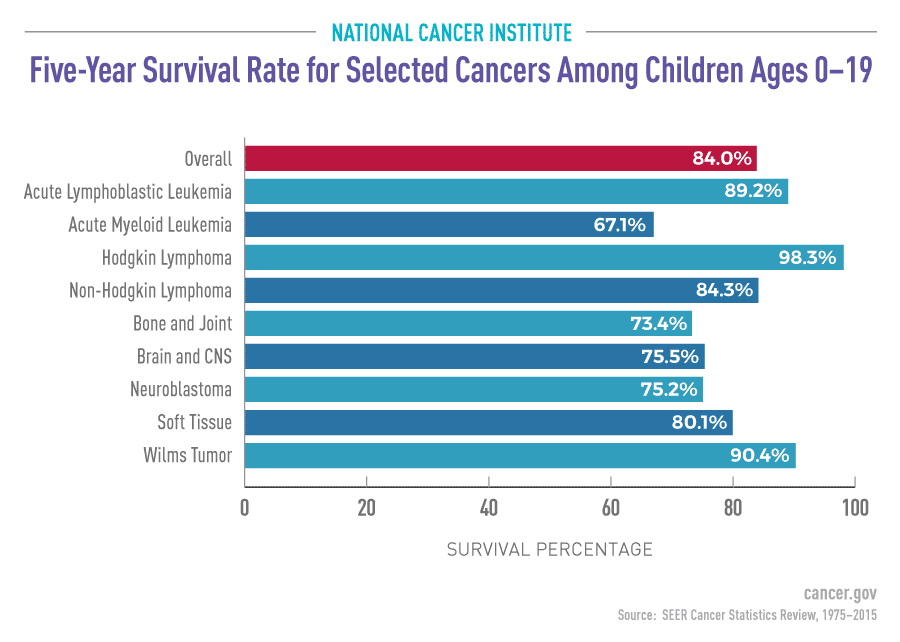
In a study published in The New England Journal of Medicine AI, researchers illustrated that the AI model could predict glioma recurrence within a year after treatment with an impressive accuracy rate of 75-89%. This marks a substantial improvement over traditional prediction techniques, which hover around 50% accuracy. By understanding the relevance of MRI scan sequences in assessing the child’s health trajectory, healthcare providers can establish more effective monitoring processes. These advancements herald a new era in pediatric cancer care where data-driven decisions replace the uncertainty of conventional methods.
Improving Children Cancer Treatment with AI Tools
The integration of AI tools into pediatric cancer treatment is beginning to demonstrate transformative results. Particularly, models designed to analyze brain imaging data enable doctors to provide personalized care tailored to an individual child’s needs. By accurately predicting areas of concern such as the risk of relapse for patients with pediatric gliomas, specialists can adjust treatment plans proactively, increasing the chances of positive outcomes while minimizing unnecessary medical interventions.
Furthermore, the implications of using AI in this context extend beyond immediate relapse prediction. AI systems can streamline healthcare processes, suggesting more accurate timelines for follow-ups based on each patient’s risk profile. This not only alleviates stress on young patients and their families but also enhances overall healthcare efficiency. As research continues to evolve, the hope is that such AI tools will become standardized in pediatric oncology, ensuring that cutting-edge technology is used to improve the lifelines of children battling cancer.
MRI Scans and Their Importance in Pediatric Cancer Monitoring
MRI scans are a critical component of monitoring pediatric cancer progression and evaluating treatment efficacy. As non-invasive imaging technology, these scans allow healthcare providers to gather detailed information about brain tumors, track changes over time, and identify potential recurrences. The integration of AI in analyzing MRI scans extends the potential of this imaging technology, making it possible to interpret the data with greater precision and accuracy. This assures that healthcare teams can react swiftly to changes in a child’s condition.
Unfortunately, the requirement for frequent MRI scans can be a source of anxiety for both children and their families. By utilizing AI tools that can reduce the number of scans needed through improved predictive capabilities, families can experience a more manageable follow-up process. Consequently, AI not only contributes to enhanced clinical insights but also to quality of life improvements for patients undergoing treatment. As technology advances, balancing effective monitoring with patient comfort will remain an essential goal in pediatric oncology.
The Future of Predictive AI in Pediatric Oncology
Looking into the future of pediatric oncology, the role of predictive AI tools appears to be vital in shaping more effective treatment arsenals against childhood cancers. As research progresses, improvements in AI’s ability to analyze data—from imaging to genetic profiles—will likely usher in a new era of precision medicine. This would mean that treatments can be tailored not just to the type of cancer, but also to the specific biology of the patient, thus maximizing treatment success while minimizing side effects.
The vision is to leverage AI progressively to support clinical trials that assess the real-world functionality of these intelligent prediction models in diverse environments. By implementing predictive AI in routine clinical practice, healthcare providers could ensure that children receive timely interventions and avoid the harrowing consequences of treatment delays. Cultivating these innovative solutions will pave the way for a more hopeful future for children battling cancer.
Challenges Ahead for AI in Pediatric Oncology
Despite the promising advancements AI brings to pediatric oncology, significant challenges remain. Integrating predictive AI tools into existing healthcare frameworks requires comprehensive validation across a wide variety of clinical settings. Continuous adaptation and professional training are essential to ensure that healthcare practitioners can effectively utilize these sophisticated systems. Moreover, ethical concerns regarding data privacy and AI decision-making must be thoroughly addressed to foster trust among patients and their families.
Additionally, striking a balance between technological advancement and the human aspect of medicine will be crucial. While AI can enhance predictive accuracy, the compassionate care that pediatric patients require during challenging times must never be overshadowed. Ensuring that innovations in AI serve to empower and improve patient care, rather than replace the human touch, will be key to successful integration into pediatric oncology.
AI and Collaborative Efforts to Combat Pediatric Cancer
The battle against pediatric cancer encompasses the need for collaboration among researchers, healthcare providers, and technology experts. With advancements in AI technology, interdisciplinary partnerships are vital in developing responsible AI tools that will drive better outcomes for children. Collaborative efforts can leverage diverse expertise and resources, enhancing the effectiveness of predictive AI tools in identifying cancer recurrence risks and understanding complex tumor behaviors in children.
Moreover, research initiatives that unite institutions can facilitate data-sharing opportunities, allowing AI algorithms to learn from a broader range of cases. These collective endeavors can help ensure that predictive AI in pediatric oncology retains clinical relevance. By working together, collaborators can create a comprehensive ecosystem aimed at combating pediatric cancers, ultimately ensuring that every child has access to the best possible care tailored to their unique needs.
Parental Perspectives on AI in Pediatric Cancer Treatment
The incorporation of AI into pediatric cancer treatment can have profound implications for families grappling with such a challenging diagnosis. Parents often seek reassurance and guidance as they navigate their child’s treatment journey. AI tools that provide accurate predictive insights can help parents make informed decisions regarding their child’s care, understanding the likely outcomes and necessary interventions. By demystifying the treatment process, parents may experience less anxiety and greater confidence in their child’s medical team.
However, as AI becomes increasingly prevalent in healthcare decision-making, it is crucial for providers to maintain open lines of communication with families. Educating parents about how predictive AI tools function and the facts behind their effectiveness can foster trust and acceptance. When parents feel empowered with knowledge about their child’s care, they are more likely to advocate for their best interests, thus promoting a cooperative relationship with healthcare providers.
The Impact of Early Detection through AI on Pediatric Cancer Care
AI’s ability to enhance early detection of pediatric cancers represents a breakthrough in patient care that promises to significantly improve survival rates. By identifying cancerous changes swiftly and with accuracy, predictive AI tools can prompt earlier intervention, which is crucial in affecting treatment outcomes favorably. For instance, methodologies that analyze longitudinal imaging data empower clinicians to make proactive choices, intervening at strategic points in a child’s care pathway to reduce the burden of disease and treatment.
The reduction of diagnostic delays directly translates into more favorable prognoses, as early treatment can prevent the progression of the disease. The ripple effect of these early interventions could lead to a generation of children receiving prompt, often less invasive treatments, further enhancing their quality of life. Evaluating and validating these approaches will be essential as AI continues to carve out a prominent role in pediatric oncology.
Frequently Asked Questions
What is the role of AI in pediatric oncology for predicting cancer recurrence?
AI plays a crucial role in pediatric oncology by leveraging advanced algorithms to analyze MRI scans over time, significantly improving the accuracy of predicting relapse risk in children with brain tumors, particularly gliomas. Traditional methods often fall short, but AI tools can synthesize data from multiple scans, thereby providing more reliable predictions for treatment planning.
How does AI improve the prediction of glioma recurrence risk in children?
AI enhances the prediction of glioma recurrence risk through a technique called temporal learning, which evaluates multiple MRI scans taken over specific time intervals. This approach allows the AI model to detect subtle changes in the brain that may signal a higher risk of relapse, achieving an accuracy rate of 75-89%, compared to about 50% with traditional single-scan methods.
What are predictive AI tools and how do they benefit children receiving cancer treatment?
Predictive AI tools are advanced software systems that analyze medical images and patient data to forecast potential health outcomes, such as cancer recurrence. In pediatric cancer treatment, these tools help identify high-risk patients early, thereby allowing for more tailored and proactive treatment strategies, potentially reducing the need for frequent imaging and improving the overall care experience for children.
Why are MRI scans important in the context of pediatric cancer prediction?
MRI scans are vital in pediatric cancer prediction as they provide detailed images of the brain, allowing healthcare professionals to monitor changes over time. In the context of AI, these scans serve as critical data points that enable predictive models to assess glioma recurrence risk, leading to more informed treatment decisions and potentially better outcomes for child patients.
How can pediatric cancer prediction impact treatment decisions for children with gliomas?
Pediatric cancer prediction, particularly through AI-driven analysis of MRI scans, can significantly impact treatment decisions by identifying which children are at the highest risk for glioma recurrence. This information can lead to more personalized treatment plans, such as reducing the frequency of follow-up imaging for low-risk patients or initiating early intervention strategies for those identified as high-risk.
| Aspect | Details |
|---|---|
| Study Focus | Pediatric cancer recurrence prediction using AI vs. traditional methods |
| AI Tool Description | An AI tool that analyzes multiple MRI scans to predict relapse risk more accurately than single-scan methods. |
| Study Findings | 75-89% accuracy in predicting recurrence using a temporal learning approach, superior to 50% accuracy of traditional single-scan methods. |
| Methodology | Temporal learning takes multiple scans over time to improve prediction accuracy, training the AI to recognize changes over time. |
| Future Implications | Potential for launching clinical trials and reducing unnecessary imaging for low-risk patients, while targeting high-risk ones early. |
| Study Support | Research funded in part by the National Institutes of Health and involved collaboration across institutions. |
Summary
Pediatric cancer prediction, particularly concerning the recurrence of tumors like gliomas, has advanced with the introduction of an innovative AI tool. This AI tool enhances the ability to predict relapse risks more effectively than traditional imaging methods, which is a significant breakthrough for improving the future care of pediatric patients. The emphasis on using multiple brain scans through temporal learning signifies a noteworthy step towards more personalized and accurate management of pediatric cancer, ultimately aiming to alleviate the stress of repeated imaging on young patients and their families.